Massage therapy and physical pain are kind of besties—well, more like frenemies, maybe. We often think of them together and we get excited about massage therapy’s potential to address and lessen pain, but we forget that pain is just one of many experiences.
When it comes to people with serious health conditions and the people who love them, pain might be a feature of their experience, but the benefits of massage therapy go far beyond addressing this single symptom.
Let’s start by ensuring we’re using the same definition of massage therapy. We know this is a topic of significant debate, but for the purposes of this article, we will use the following definition:
Massage therapy consists of the application of massage and non-hands-on components, including health promotion and education messages, for self-care and health maintenance; therapy, as well as outcomes, can be influenced by: therapeutic relationships and communication; the therapist’s education, skill level and experience; and the therapeutic setting.1
Fully grasping the potential value of massage therapy, as defined above, for people affected by illness requires that we understand the deep truth that massage therapists are so much more than hands.
Our words, our body language, our ability to notice and limit the impact of bias on our client interactions, and more make up this thing we call “therapeutic relationship,” which lies at the root of our ability to decrease anxiety, increase a sense of peace and facilitate an experience of transcendence.
In this article, we’d like to invite you to consider the impact of those harder-to-express benefits that so many people enjoy from massage therapy but which get very little public appreciation and even less focus in research. Aspects like emotional well-being, decreased isolation and improved coping can be game changers for people living with serious health conditions.
Destigmatizing “relaxation.” How many times have you heard the phrase, “Just relaxation massage” as though the “brand” of massage that delivers relaxation is less valuable or legitimate than other types of massage? As a profession, we have downplayed, undersold and essentially ignored the deeply important therapeutic significance of relaxation.
There is a worthwhile body of research2,3,4 that explores the experience of both patients and caregivers beyond the quantitative measures of pain and anxiety. Relaxation is key to those experiences.
Well-being is another word that has essentially lost its meaning in modern language, but the authors of this article feel confident that massage therapists have the potential to profoundly impact well-being in the lives of people affected by serious illness.
When we talk about quality of life, we’re talking about well-being. When we talk about having less pain, that’s also about well-being. When anxiety and depression feel less pressing, less heavy, less suffocating—these are all aspects of well-being, and they are not individual.
They are all pieces of what make up any one human’s (and every human’s) experience. And they can all be facilitated by massage therapists with the right tools.
Cancer: Massage + Cancer-related Distress
Byron (not his real name) believed entirely in his own agency and ability to control his fate—until he received a cancer diagnosis. In that moment, he felt as if his entire identity collapsed into one unwanted label: Cancer Patient.
A lifelong entrepreneur, Byron suddenly felt that all his future projects became impossible in the face of this diagnosis. In his mind, his world shrank to the size of the errant cells in his body, and all his resources (physical, emotional and financial) could only flow into his cancer treatment.
In addition, as a person of color in the U.S., Byron already had many experiences of being ignored, mistreated and dismissed by medical professionals. As a result, he found it difficult to trust the system to care for him. What followed for Byron was a period of significant depression as he struggled in the face of his diagnosis. For Byron, a cancer diagnosis included cancer-related distress.
Cancer-related distress affects almost every person diagnosed with cancer at some level, with about 40% of patients reporting “notable distress,”5 which is defined by the National Comprehensive Cancer Network as “a multifactorial unpleasant experience of a psychological (i.e., cognitive, behavioral, emotional), social, spiritual and/or physical nature that may interfere with one’s ability to cope effectively with cancer, its physical symptoms, and its treatment.”5
Anxiety and depression are the most prevalent mental health challenges that accompany distress. Patients report the most frequent sources of cancer-related distress as worry (55%), fatigue (54%), fears (45%), sadness (44%), pain (41%) and sleep disturbance (40%).6
Distress can appear in anyone faced with a cancer diagnosis, and it is important to note that social factors can serve to increase or mitigate the experience of cancer-related distress. For example, distress is often associated with lower income or lack of access to health insurance.
Working with people who are in or have been through cancer treatment requires training beyond our foundational education. Oncology Massage training of at least 24 hours is the minimum standard.
In Oncology Massage training, we learn to understand more about the disease of cancer itself, as well as develop and practice the clinical reasoning skills we need to adapt a massage for the effects of cancer and cancer treatment.
Without this training, we run the risk of causing both immediate and lasting harm and, as important, we miss the opportunity to be of specific and valuable service to the people we touch.
Beyond the hands-on adaptations and technical knowledge, we also need deep self-reflection and emotional regulation skills when working with people affected by serious illness. As humans, we may have personal experience with cancer or with caring for a loved one during their treatment.
That does not qualify us to provide safe, accurate massage therapy for someone affected by that illness. We all have our own fears and assumptions about illness.
We must remain aware of the history that we carry into the treatment room. Our challenge becomes remaining curious and open in the face of whatever shows up in our space, even if it “looks like” something we think we know.
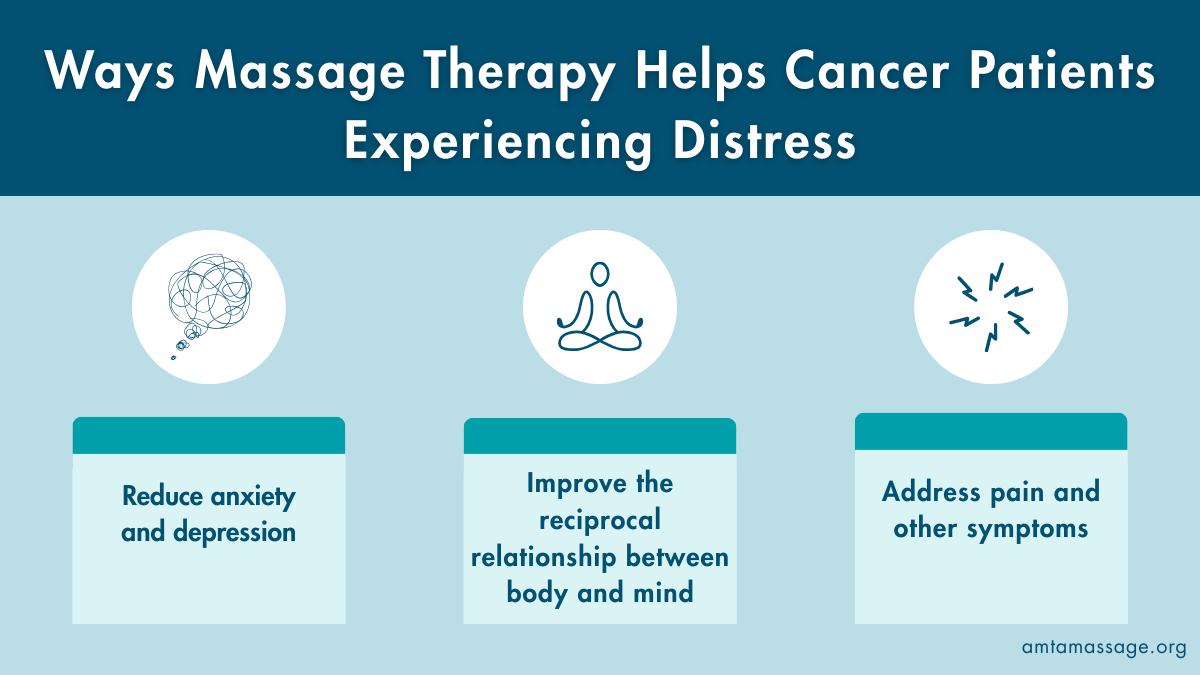
With the proper education, there is much we can do to improve the day-to-day quality of life for people faced with a cancer diagnosis. The ways in which massage therapy may help cancer patients experiencing distress include:
- Reduce anxiety and depression: reductions of anxiety and depression are massage therapy’s most commonly reported effects, with a course of treatment providing benefits similar in magnitude to those of psychotherapy.6
- Improve the reciprocal relationship between body and mind: massage therapy can link changes in the tissue to changes in the recipient’s cognitive self-awareness.6 As a nervous system-based intervention, massage can help recipients reconnect their body into a whole.
- Address pain and other symptoms: Massage therapy can be an effective treatment for pain,6 but can also reduce fatigue, stress, anxiety and nausea.6
Autoimmune Conditions: The Invisible Cost
Roughly 1 in 15 people in the U.S. has an autoimmune disease. It’s no surprise that, with more than 100 identified autoimmune diseases, these diagnoses cover the spectrum with just about any tissue or organ in the body potentially being affected.7
The common nature of these conditions leads to a sense of normalization that is unhelpful. We all likely know at least one person with rheumatoid arthritis, lupus, psoriatic arthritis, Crohn’s disease, type 1 diabetes or multiple sclerosis.
Unless we know this person well, however, we likely almost always see them “at their best,” when they feel well enough to be out in the world interacting. That doesn’t give us a very real view into what it’s like to live with these conditions.
Mental health challenges are common among people who live with autoimmune diseases. A 2013 study in Denmark8 found that participants (who all had autoimmune conditions) were 45% more likely to develop anxiety or depression, and the Cleveland Clinic reports that as many as 50% of people with MS have clinical depression.9
People living with type 1 diabetes often develop cognitive deficits across their lifespan that affect attention, information processing speed and executive functions, as well as depression, anxiety and decreased quality of life.10
In their 2018 paper, “Depressive Syndromes in Autoimmune Disorders of the Nervous System,” Drs. Liu and Tang discuss “pleasure loss” and “sleep disturbance” as common aspects of depressive presentation in people with autoimmune conditions.11
Living with or caring for someone who lives with an autoimmune condition means your life is significantly disrupted. There is worry and fear about changes in disease progression or severity, flare-ups, as well as endless and sometimes seemingly pointless medical appointments.
Many people feel stigmatized and isolated by their illness, and many of these conditions come with chemical and hormonal changes that can be unpredictable and hard to manage. Changing health status and changing energy levels can lead to one’s life feeling smaller.